August 8, 2023
Article/research/presentations of interest below:
1) With limited research on the impact of New York’s two sites for supervised use of illegal drugs, hard data to support either success or failure is still scarce. It’s an experiment, and the whole country is watching to see if New York City’s approach to preventing overdoses works. No pressure.
———————————–
2) Last month, David de Voursney, Director of Systems and Services Improvement at SAMHSA facilitated a presentation for association directors across the country during a National Council Association Execs meeting. Mr. de Voursney is often referenced when I speak to NY state agency leads as they continue to interact with SAMHSA re: New York’s CCBHC Demo Program, and the Expansion Grant Program. I have attached the presentation de Voursney reviewed with participants, fyi.
————————————
3) An analysis of new federal data revealed that only one in five adults who had opioid use disorder (OUD) in 2021 received medication to treat it. People who received treatment through telehealth were about 38 times more likely to receive medication for OUD (MOUD) than those who were not treated virtually for any reason. And, there were disparities in who received MOUD. White adults were 14 times more likely than Black adults to receive medication, and there was a similar gap between working and unemployed adults. Men were six times more likely than women to get medications, and those in urban areas were three times more likely than those in non-urban areas. (Articles here, here, and here; Study here)
——————————-
4) There is an urgent need to prioritize and expand substance use disorder (SUD) treatment resources, including comprehensive rehabilitation programs, counseling services, harm reduction strategies, and access to medication for addiction treatment (MAT). Doing so requires a multifaceted approach involving various strategies. In this week’s blog, Senior Director Eric Bailly shares seven of the most effective ways to enhance access to SUD treatment, including integrated care and insurance coverage and parity. Check out his blog to learn more about these strategies, and the other five. (Blog here)
———————————–
5) Interesting article from OpenMinds:
| The Addiction Treatment Best Practice Question |
|
August 7, 2023 | Monica E. Oss, OpenMinds
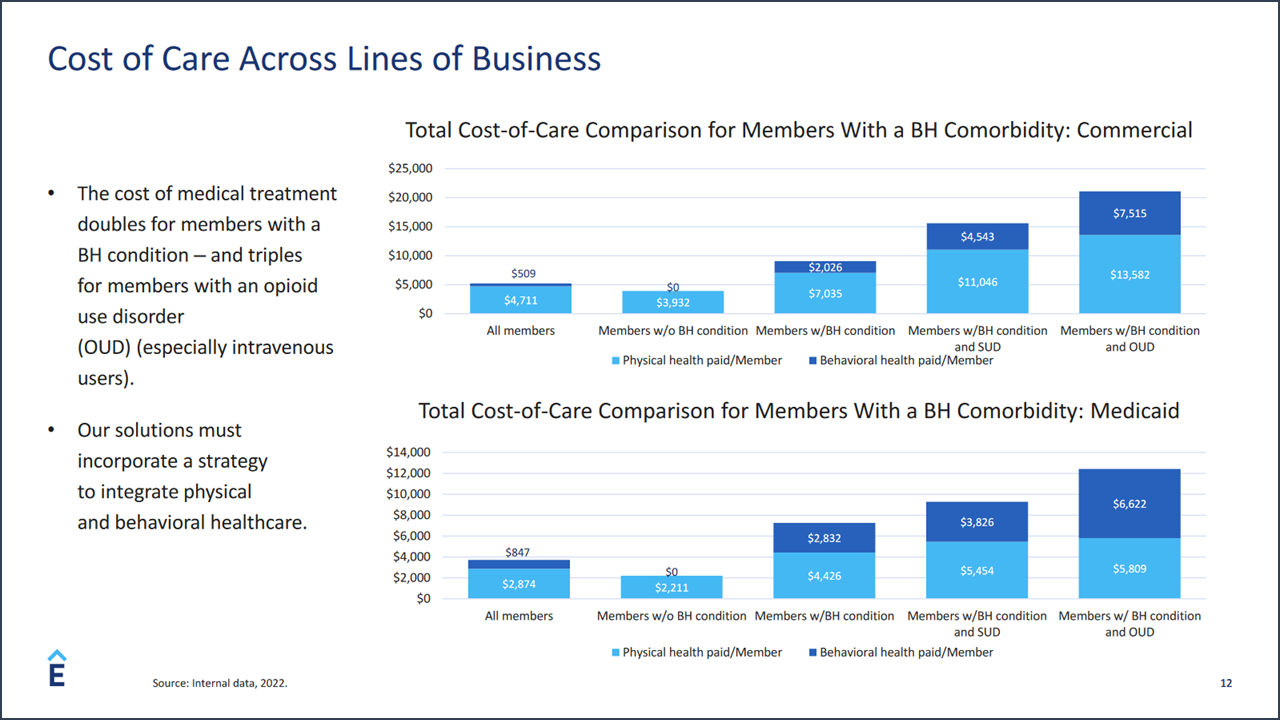
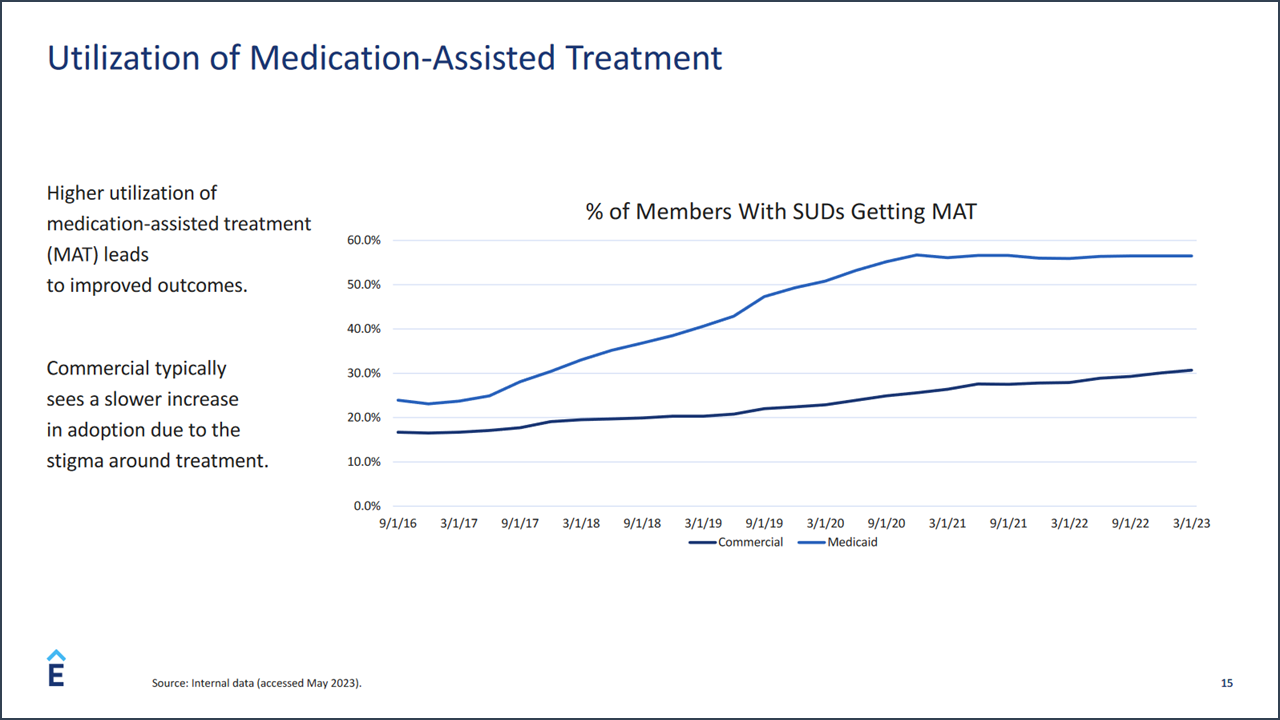
I was surprised to learn that the use of medication-assisted treatment (MAT) for addiction treatment in members of commercial health plans is significantly less than use of MAT among Medicaid health plan members. That was a key takeaway from the recent keynote session lead by David Lederman, Senior Product Manager for Elevance Health, I had assumed that use of these medications, accepted ‘best practice’ in the addiction treatment, would be greater among the population of commercial members. According to Mr. Lederman, the 20+% difference in utilization between the two populations can be attributed to a number of factors including preconceived notions about the medications and the difference in treatment provider organization philosophies. At the same time, treatment for addictions in Elevance Health’s affiliated plan population still skews heavily toward inpatient and residential levels of care. Residential and inpatient care accounts for more than 50% of spending for Medicaid members and 59% for commercial members. The lower uptake of MAT-focused treatment and the use of inpatient and residential level of care is a key clinical and finance concern for management of Anthem’s commercial health plans. Elevance Health’s claims data indicates that behavioral health treatments account for the sixth highest spending category for its commercial population. The cost of medical treatment doubles for members with a behavioral health condition—and triples for members with an opioid use disorder (OUD), especially intravenous users, a 77% higher total cost of care than the average member.
This landscape in addiction treatment has led Anthem to rethink its addiction treatment network and its capabilities. On the MAT side, Anthem is committed to doubling MAT use and has eliminated prior authorization requirements, according to Mr. Lederman. Elevance Health is also focused on finding community-based treatment models with integrated physical/addiction treatment services. With this approach, the company is focused on a few key performance measures—rapid access, quality of care, provider experience, and consumer experience. Two early initiatives have had positive returns. First, they have used predictive analytics to identify and engage members with addictions. Members get a single point of contact to help manage their physical health, mental health, and addiction treatment needs. And, Anthem has set up a system with prompt access to addiction treatment appointments. The results in their Medicaid plans—a 63% reduction in hospitalizations and a nearly 40% decrease in overdoses. As Elevance Health evaluates new provider organization partners, they are looking for organizations with an individualized approach to treatment—evaluating the needs of each member to determine the most appropriate level of care and treatment approach. In addition, they are looking for organizations with demonstrated success in reducing the adverse effects of addiction, reducing overdoses and suicides. And they are looking for a great consumer experience—with measures of consumer satisfaction, consumer engagement, and Net Promoter Scores.
How does Elevance measure success? “We define outcome goals and then flesh out the corresponding KPIs,” explains Mr. Lederman. “For instance, access, quality of care, and provider and patient experience were and are critical goals intra- and post-pandemic, as demand surged and remains a challenge. The corresponding KPIs include engagement, positive measures of outpatient and intensive outpatient care, suicide intervention, cost-of-care impact (i.e., ROI), reduction in relevant utilization measures, and more. These KPIs must be relevant and measured across appropriate timescales.” For provider organization executives, there are new opportunities in enhancing the available options for consumer addiction treatment. But, like most emerging opportunities in the field, a targeted focus on a particular population and the ability to measure impact are critical. But Mr. Lederman considers the Elevance Health approach to be one of being a partner in care access for members. He said, “We should take off our project manager hats […] and work together to partner, share information, and leverage innovation to address the needs of all of our stakeholders.” |